The outbreak of an infectious disease can be overwhelming if a hospital is not prepared. Hospitals employ a variety of strategies to prevent the spread of such illnesses. One of the most prevalent approaches is to treat these patients in isolation rooms. For those working in and around isolation rooms, their safety depends on proper control of the differential pressure of the room. As the coronavirus becomes ever more a pressing concern, it is critical for hospitals and staff to take the right precautions for keeping isolation rooms safe.
What are Isolation Rooms?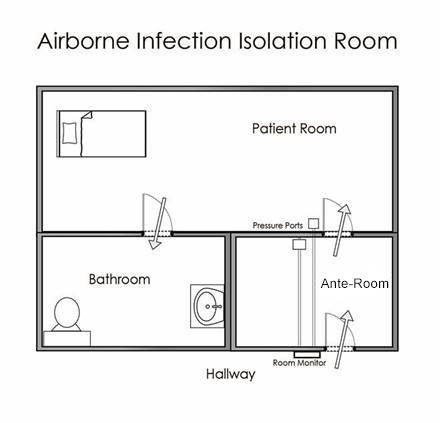
Airborne Infection Isolation rooms, commonly referred to as isolation rooms, are single occupant hospital rooms designed to contain airborne pathogens. The Centers for Disease Control (CDC) requires the use of isolation rooms to protect the public from the spread of infectious disease. Isolation rooms are also necessary to protect hospital staff from illnesses where coughing conditions pose a risk.
Isolation rooms are designed to prevent contaminated particles from spreading beyond a quarantined area. To prevent the contaminated air from escaping, isolation rooms require negative air pressure relative to the outside reference area, a difference of at least -0.01"WC. This ensures clean air is drawn into the room and contaminated particles, such as cough droplets, inside the room are not able to escape. The exhaust from isolation rooms is not recirculated into the hospital's main HVAC system; rather, dedicated ductwork filters the air through a high-efficiency particulate air filter and then moves it to ventilation stacks on the roof where atmospheric air sufficiently dilutes it.
A relevant example of an infectious disease currently being treated in isolation rooms is the coronavirus. Since coronavirus can be easily spread through the air, treating patients in an isolation room keep staff and other hospital patients safe from contracting the disease.
Common Faults of Isolation Rooms
Although an isolation room might have the equipment necessary to meet minimal safety standards, such technology is often outdated and has disadvantages that can put patients and staff at risk. In an outbreak such as coronavirus, upgrading old instruments to eliminate said drawbacks can help ensure the safety of an isolation room. Improper or unbalanced room pressurization can put patients and staff at risk of exposure if dangerous contaminants escape the space.
For decades, hot-wire anemometers have been used to measure pressure in operating rooms and isolation rooms. However, hot-wires have several inherent shortcomings that impact performance. By design, air must pass through a hot-wire to measure pressure, making the instrument highly sensitive to dust and differences in air density. Hot-wires must be cleaned and recalibrated often for proper performance but taking an isolation room offline for said cleaning is time-consuming and expensive. If a dirty sensor is not addressed, a room could potentially and unknowingly fail to meet pressure requirements and result in a failed inspection. An element of hot-wires not typically addressed is that because they require a hole in the wall for air to flow through, the room is technically not in isolation. These inherent design drawbacks can put patients at risk.
Another technology frequently used in isolation rooms with disadvantages that can affect patients is a ball pressure indicator. A ball pressure indicator uses a ping-pong ball in a plastic tube that moves to whichever room is positively pressurized. Although common and inexpensive, these devices are remarkably difficult to install properly. If the indicator is not perfectly level, it will not function properly. The isolation room can then be unsafe for patients and staff if the indicator displays the pressurization is correct when it is not. In addition, ball pressure indicators are strictly visual; if the room is not properly pressurized, the only way to know is to look at the indicator. It does not alarm or connect to a building management system (BMS), which can be dangerous for patients.
How to Better Maintain Safety of Isolation Rooms
The technology in the aforementioned paragraphs does help isolation rooms meet standards, but it is not the most effective for keeping these spaces protected. The CDC, the Facility Guidelines Institute, and the Joint Commission spent an inordinate amount of time ensuring that healthcare and lab facilities conform to isolation room requirements. Hospitals are often fiscally constrained from making facility upgrades; yet, now more than ever, does the healthcare system need to demonstrate it can handle a potential epidemic, especially as the risk of coronavirus looms.
The most resourceful way to implement an isolation room strategy is to utilize the real-time monitoring and alarm capabilities of a room pressure monitor (RPM). RPMs are the safest and most reliable monitoring solution for isolation rooms. A transducer-based pressure sensor makes it more accurate and dependable than a ball pressure indicator and requires zero manual testing. Some devices also have the ability to monitor temperature and humidity. A room pressure monitor produces both audible and visual alarms when a room has been compromised, thus reducing the labor required to ensure negative pressure and minimizing the possibility of a catastrophic oversight.
Another best practice for maintaining safety is to use transducer-based pressure sensors instead of hot-wires. Transducers are installed with pressure ports in the corridor and isolation room and therefore don't require a hole through the wall. These are much more accurate and reliable than ball pressure indicators. Typically low maintenance, they connect to a BMS or RPM for real-time monitoring.
Setra Can Help Keep You Safe
Setra has engineered the best devices to protect patients and staff, especially those in isolation rooms. Setra FLEX, the Setra FLEX Conversion Kit, and Setra Lite can help prevent airborne infections like the coronavirus from spreading.
 For isolation rooms, the most effective way to monitor room pressure conditions is with a monitor that can support multiple rooms, like Setra FLEX. In addition to monitoring room pressure, FLEX can display measurements for temperature, humidity, and air changes per hour. It can be controlled over the network via BACnet or through a BMS. With an accuracy of 0.25%, FLEX can ensure the safety of a critical space.
For isolation rooms, the most effective way to monitor room pressure conditions is with a monitor that can support multiple rooms, like Setra FLEX. In addition to monitoring room pressure, FLEX can display measurements for temperature, humidity, and air changes per hour. It can be controlled over the network via BACnet or through a BMS. With an accuracy of 0.25%, FLEX can ensure the safety of a critical space.
To combat the drawbacks of a hot-wire, Setra designed the Setra FLEX Conversion Kit. Setra uses dead-ended pressure transducers, which means no air flows through the pressure tubing. As air is a significant carrier of contaminants in a hospital, a dead-ended sensor that doesn't rely on air flowing through it for a pressure reading cannot be contaminated, nor does it require a hole in the wall to operate. With no air flowing through the sensor, Setra's transducers do not require the unreasonable maintenance required by outdated hot-wire anemometers. The Setra FLEX Conversion Kit replaces hot-wire anemometer-based room pressure monitors in only 20 minutes without any construction necessary.
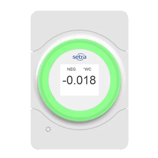
Setra Lite can replace outdated and unreliable technology like a ball pressure indicator or pressure gage. Using Setra's dead-ended capacitve transducers, Lite allows staff to see at a glance if a room is properly pressurized, even from down the hall. Unlike the visual-only function of a ball pressure indicator, Lite's analog output can be directly connected to a BMS or Setra FLEX to indicate when a room goes into alarm.



